Most people expect parenthood to be the most exciting and fulfilling experience of their lives. Even though they realize (or soon find out) that babies bring challenges, they expect to overcome those and raise a happy, healthy family.
But for some unfortunate couples, difficulties arise early on, before they have had time to savor even a moment of joy. My friend Natalie has graciously agreed to share the story of how her introduction to motherhood was far from what she expected, an experience shared by too many women. She calls her account
A Mother’s Sorrow: Battling Postpartum Depression
(I have interspersed questions and answers about childbirth and depression throughout her story, to add context. You’ll recognize these by the ? marks. )
Natalie writes..
From the moment a woman sees those two thin blue stripes on a pregnancy test, her world is turned upside down. There’s joy and panic rushing through her mind as she struggles to come to terms with what’s happening.

When the time is right, she calls and texts her friends and family and there’s congratulations all around. Some offer advice and make tongue-in-cheek jokes about parenthood, but in the end assure her mostly joy awaits .
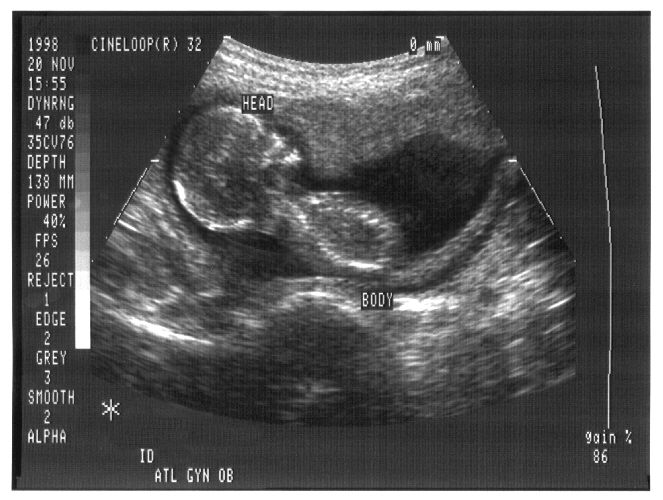
Appointments come and go as she gradually gets to know the life growing inside, kicking and dancing to the sound of her voice. The nursery comes together, and she and her spouse feel the deepest excitement for the approaching arrival of their little girl, Emma.
This was the beginning of my journey into motherhood and the foundation of the most excruciating part of my existence to date.
at the hospital for labor …
I woke up one December morning feeling my water break as I stood up from bed. Within the hour my husband came home from work to take me to the hospital where I underwent an uneventful labor up until the last few hours.
Then the nurses realized Emma’s heart rate was dropping with each contraction. They did everything they could to speed things up without putting further stress on her, but when they asked me if I would consent to an emergency cesarean operation I didn’t hesitate. I wanted them to save her, no matter what.
What is a cesarean birth?
Cesarean delivery, also called c-section, is surgery to deliver a baby. The baby is taken out through the mother’s abdomen. Most cesarean births result in healthy babies and mothers. But c-section is major surgery and carries risks. Healing also takes longer than with vaginal birth.
Most healthy pregnant women with no risk factors for problems during labor or delivery have their babies vaginally. Still, the cesarean birth rate in the United States has risen greatly in recent decades. Today, nearly 1 in 3 women have babies by c-section in this country. The rate was 1 in 5 in 1995.
and delivery
Further numbing agents were administered and I felt the immediate fatigue from the anesthetics, but I was still conscious during the operation. From the moment the blue curtain was draped over my chest, I felt like half of my body was in a separate room. I couldn’t feel or see anything other than a constant tugging.
It was early evening two days later when my doctor announced her birth, offering a brief glimpse of her before they whisked her off to the nursery.
My husband was still with me at that point and I remember vividly asking him and everyone around me how much she weighed and what color her eyes were. Nobody would answer me. Eventually a nurse asked my husband to follow her and I was left alone with the nurses who still wouldn’t answer my questions. To this day, my husband denies I said word, but I did mumble. Evidently the anesthetic kept me from communicating.
meeting my baby-but no “magic”
Back in the recovery room they formally introduced me to my little girl, but the drugs were still in my system, so I needed help holding her. And this is where my struggle began. For the longest time, my doctor believed it to just be a case of the baby blues, but I knew at that moment…what was meant to be a magical moment…that something was amiss.
The little girl in my arms was beautiful, listened to my voice, had my eyes, but somehow felt like an uninvited guest to me. After 36 hours of labor, I expected there to be more pomp and circumstance behind our special meeting. That’s how my own mother and all my friends had described it. I knew nothing of what was going on in my head, but I was deeply repulsed by my lack of affection towards her.
Mothers-to-be often spend so much time in anticipation of labor, they don’t think about or even know what to expect during the first hours after delivery.
womenshealth.gov
“failing at being a mother”
During the next few weeks things worsened for me. The sleepless nights and chaos of welcoming a newborn into our home took its toll on my emotional state. The stress combined with the surgical delivery made it difficult for me to produce enough milk to breastfeed – something I had set my heart on months before.
Delivering around the holidays complicated getting assistance from lactation consultants who were on leave. I felt my world was crumbling around me and each day I was failing more and more at being a mother.
I addressed this at each follow up appointment with my doctor, who decided to monitor things further before introducing me to the chemical-altering world of antidepressant medication. I was told it could be a severe case of the baby blues, which could take up to a couple of months to pass.

What are baby blues?
Many new mothers feel blue after giving birth, feeling sad, weepy, and overwhelmed for a few days. Changing hormones, anxiety about caring for the baby, and sleep loss all can affect emotions.
Doctors consider these feelings normal and expect them to disappear in a couple of weeks. If they persist longer than two weeks, or suddenly become more severe, the new mom should see her doctor for evaluation. It may be something more serious, as it turned out to be for Natalie.
“I can’t”
I lost my appetite. My parents came over to offer words of wisdom and comfort and allowed me to spend the night to get rest several times, but I would still cry through our talks and cry myself to sleep at their house. Each time I heard someone say, “it gets better” or “you’ll develop a bond with her”, I felt empty, numb, and hopeless.
I felt a grief that I can’t fully describe. I felt an agonizing sorrow in the pit of my stomach as though I had lost a loved one. I would try to feed Emma only to end up frustrated, so my husband would take her and tell me to rest. It was in these moments that I would cry uncontrollably, for hours and hours with voices in my head constantly telling me “I can’t”.
the crisis-contemplating suicide
It was these feelings of uselessness which drove me to call my doctor telling her I contemplated suicide. I had already told my husband to hide my gun and assured all my loved ones that I never considered harming anyone other than myself.
My doctor finally agreed that this was not the baby blues and had me come in the next day for an evaluation, where I overwhelmingly passed the indicators for PPD- postpartum depression.
What is postpartum depression?
In postpartum depression, a mother feels such intense feelings of sadness, anxiety, and despair that she has difficulty taking care of herself and her infant. It usually starts within three weeks of delivery but can be anytime up to a year after delivery.
Multiple factors contribute to the development of postpartum depression including a prior history of depression, hormone changes, fatigue due to lack of sleep or a caesarean delivery, and stress such as an infant with medical problems, financial difficulties, lack of family support, marital discord, or recent family death.
receiving a medication- and hope
I received a prescription for escitalopram, the fastest acting antidepressant on the market, and was told to come in every two weeks until I had reached the target dosage for treatment. Within the first 72 hours of treatment my family noticed a difference in my behavior.
It was the first time in months they’d seen me smile and laugh. I finally felt a glimmer of hope as I was able to feed and change Emma without breaking down in tears. A month went by and life became enjoyable for the first time since my baby’s birth.
What are antidepressants?
Escitalopram is one of several medications called SSRIs, selective serotonin reuptake inhibitors, that are effective for all kinds of depression. They work by increasing the levels of the hormone serotonin in the brain, which regulate mood. After starting an antidepressant, a woman should feel better within 3-4 weeks.
a setback quickly resolved
Then the four-month sleep regression came. After weeks of Emma sleeping in her own crib through the night, she suddenly began screaming for hours on end and I felt that familiar sense of darkness creep back into my life. Yet again, I had to rely on my husband’s resolve to make it through the night.
Again, I felt incapable and less than what they both deserved. Knowing that I was already getting assistance from my new medication, this seemed to hit me even harder than before. I felt as though I would never get the help I needed to keep my mind focused on the positive.
I thank God I had the self-awareness to contact my doctor immediately, who prescribed twice the dosage within 12 hours of me sending the email. Though the sleep regression was difficult, the stronger medication allowed me to act as the mother I was meant to be.
I no longer had to sit idly by and watch my husband rock her to sleep and feed her most of the time. I developed confidence in myself and began to kindle a bond to my daughter for the first time.

relishing the joy of motherhood
As she cried in the dark at 3 am one morning, I could see the world through her eyes. She simply wanted warmth and love – something I was unable to provide those first four months. I could have fallen into yet another bout of despair over how I neglected her but instead I simply lived in the moment and held her close.
Feeling her tiny hand caress my cheek as she drifted back to sleep and listening to her breath whispering from between her pursed lips, I made myself comfortable and sat there for hours taking in her scent and relishing my ability to enjoy our time together when I would rather be in bed.
healing painful memories
Months have passed and Emma is now approaching her first birthday. I’ve delayed finishing this story since I’ve wished to put this all behind me, having no desire to relive those memories. That I’m now able to finish what I started is a sign of healing.
The memories of my so-called “failures” are what I now hold dear as my greatest triumphs. I can overcome the stigmas of being unable to breastfeed and unwilling to care for my own child in her first few weeks of infancy.
rejecting the stigma of post partum depression
While society’s norms lead us to believe this is unacceptable with no exceptions, I pray that this story makes its way to a few young women who desperately need to know that it is more than okay to feel these emotions after bringing a life into the world.
Doctors and therapists could go on for hours drowning you in information as to what goes on both physically and chemically postpartum, and they would all agree with me that it is completely acceptable to experience these stigmas I mentioned.

Natalie’s advice to new moms
Know that just because you were taught from a young age that an infant needs love and attention from her mother does not mean that mother is not allowed to adjust, to rest, and to mourn her old life.
Know that it is your very right to feel these emotions plowing through your head, just as it is your right to expect support from those around you to b e the amazing mother you already are.
Know that your baby will hold nothing against you and that nature has a majestic way of developing a bond between mother and child, no matter the obstacles.
Know that you are not alone, and that help is everywhere.
a new treatment option
With her next pregnancy Natalie plans to ask her doctor about the first and so far only FDA approved treatment specifically for postpartum depression, brexanolone.
This approval marks the first time a drug has been specifically approved to treat postpartum depression, providing an important new treatment option.
Because of concerns about serious risks, including excessive sedation or sudden loss of consciousness during administration, Zulresso (brexanolone) has been approved with a Risk Evaluation and Mitigation Strategy (REMS) and is only available to patients through a restricted distribution program at certified health care facilities where the health care provider can carefully monitor the patient.”
Tiffany Farchione, M.D., acting director of the Division of Psychiatry Products in the FDA’s Center for Drug Evaluation and Research.
resources for help
ACOG, the American College of Obstetricians and Gynecologists offers this information about
Postpartum Depression
The Office on Women’s Health from the U.S. Department of Health and Human Services published this resource on
Common Breastfeeding Challenges
Postpartum Support International
Postpartum Support International (PSI) is the world’s leading non-profit organization dedicated to helping women suffering from perinatal mood and anxiety disorders, including postpartum depression, the most common complication of childbirth. PSI was founded in 1987 to increase awareness among public and professional communities about the emotional difficulties that women can experience during and after pregnancy. The organization offers support, reliable information, best practice training, and volunteer coordinators in all 50 U.S. states and more than 30 other countries around the world. Working together with its volunteers, caring professionals, researchers, legislators and others, PSI is committed to eliminating stigma and ensuring that compassionate and quality care is available to all families. To learn more about PSI, call 800-944-4PPD or visit www.postpartum.net.
(listed for your information only, does not imply affiliation or endorsement by this blogger)
exploring the HEART of reproductive health
Thank you for reading Natalie’s story. We belong to a national women’s service organization which sponsors a yearly essay contest; Natali entered this story in the health category. You won’t be surprised to learn it won on the state, regional, and national level. She read her essay during the national convention in 2020, done virtually due to the pandemic.
Dr. Aletha
some previous posts to review
Books about having babies
Taking Charge of your Fertility The Definitive Guide to Natural Birth Control, Pregnancy Achievement, and Reproductive Health by Toni Weschler This new edition for the twentieth anniversary of the groundbreaking national bestseller provides all the information you need to monitor your menstrual cycle–along with updated information on the latest reproductive technologies. Are you…
Having a baby A to Z for mom and dad- some books to consider
In a previous post I shared books about pregnancy and childbirth aimed at women. Now I offer one that addresses the challenges of fatherhood,



So much thanks to Natalie for sharing her story and her experience. Post partum depression is a very real and very scary thing. I had a mild case after the birth of my first child and while I cannot relate to full blow post partum depression, I can relate very much to severe depression in general . It is so important for us all to share our stories of struggle and success so that we can remove the stigma attached to all mental health issues. I appreciate that you have used your platform to spread awareness and educate others on very important topics! Thanks so much for linking with me!
Shelbee
http://www.shelbeeontheedge.com
LikeLike
It was my pleasure to share Natalie’s story on your site. She and I both hope many families are helped by what she and I learned from her experience.
LikeLike
This sounded so much like my own experience. I am so sorry that you went through this. But I am glad that you got the help that you needed.
LikeLike
I’m sorry for your experience, I hope you’ve received also.
LikeLike
I too, experienced this when I had my first child. It’s such a change having a child, and I don’t think I was able to embrace it like some mothers. I saw my husband getting up in the morning and showering and leaving, and I resented that. We were much more equals before we had a baby, and suddenly, I was stuck in this job, making no money, and yet I felt like I had to make myself useful, like cleaning. I didn’t know how to be a mom, and it’s the hardest job I’ve ever done. cheers.
LikeLike
Lana, I’m so sorry you experienced this pain, thank you for sharing it with us. Yes, motherhood is a hard job, I still find it hard and I’ve been at it 41 years. I hope it’s going better for you now and you’re enjoying some of the rewards of parenthood.
LikeLike