This information is current as of the date of original publication or update. It may have changed by the time you read this. I invite you to fact-check what you read here.
Please do not use this information for diagnosis or treatment purposes. Before making health decisions, discuss with your physician or other qualified healthcare provider.
National Diabetes Month
November is National Diabetes Month, designated to raise awareness of diabetes. Taking steps to prevent or manage diabetes may lower your risk of developing health problem related to diabetes.
Diabetes is a disease that causes too much of the body’s blood glucose, also called blood sugar, to accumulate in the bloodstream. Glucose is your body’s main source of energy. Glucose comes from the food you eat, and your body can make it.
Insulin, a hormone made by the pancreas, helps glucose get into your cells to be used for energy. If you have diabetes, your body doesn’t make enough—or any—insulin, or doesn’t use insulin properly. Without insulin, glucose doesn’t reach your cells.
Diabetes isn’t just about the pancreas. Diabetes affects the eyes, kidneys, nerves, skin, and heart. Diabetes is also linked to some types of cancer.
Knowledge plus action can prevent diabetes health problems.
Stats to Know about Diabetes
As of 2019, 37.3 million people—or 11.3% of the U.S. population—had diabetes.
More than 1 in 4 people over the age of 65 had diabetes.
Nearly 1 in 4 adults with diabetes didn’t know they had the disease.
About 90% to 95% of diabetes cases are type 2 diabetes.
Know About Pre-diabetes
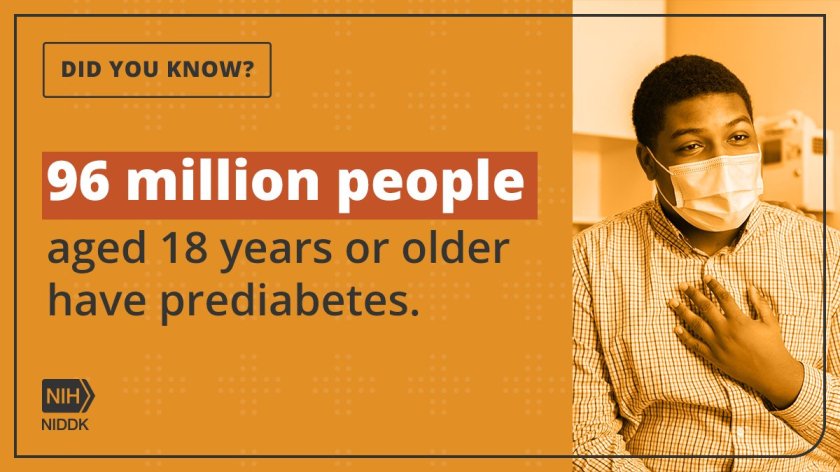
Prediabetes is defined as a blood sugar level that is in the higher end of the normal range, but not high enough to diagnose diabetes. While many of these people don’t develop diabetes, it does indicate a higher risk, so is worth knowing about and checking regularly.
Since 2001, the National Institutes of Health (NIH)-sponsored Diabetes Prevention Program (DPP) research study has shown that intensive lifestyle interventions and select medications are cost-effective in preventing or delaying the onset of type 2 diabetes in adults with prediabetes.
Learn Your Risk for Diabetes.
You are more likely to develop type 2 diabetes if you have overweight or obesity; are age 35 or older; have a family history of diabetes; are African American, American Indian, Asian American, Hispanic or Latino, or Pacific Islander; are not physically active; or have prediabetes.
The exact reasons these factors increase the chance of diabetes is not known. Scientists suspect genetics plays a role. Lifestyle may also impact one’s risk.
Later in this post you can discover your risk for diabetes with a simple online test.
The ABCs of Diabetes
Manage your blood glucose, blood pressure, and cholesterol levels.
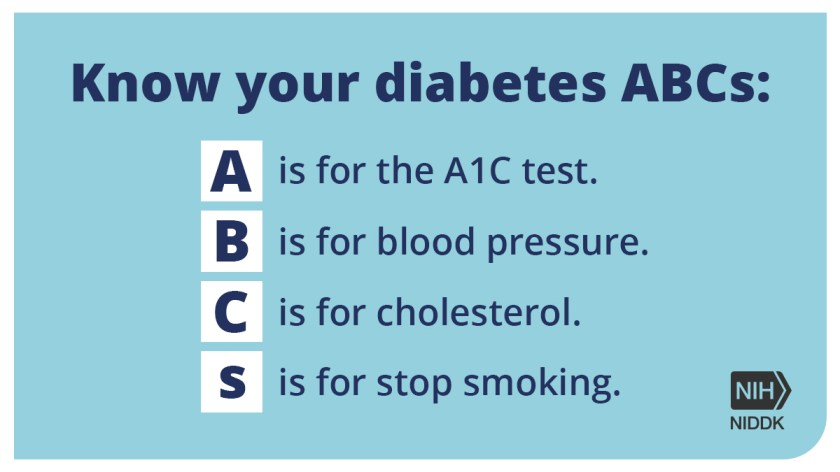
Preventing diabetes or managing diabetes as soon as possible after diagnosis may help prevent diabetes health problems. You can start by managing your diabetes ABCs.
A is for the A1C test (hemoglobin A1C) that health care professionals use to measure your average blood glucose levels. Some people with diabetes also use devices to track their blood glucose throughout the day and night.
- B is for Blood pressure.
- C is for Cholesterol.
- S is for Stop Smoking
Ask your health care team what your ABCs goals should be.
Develop a Healthy Lifestyle
Lifestyle habits like planning healthy meals, being physically active, getting enough sleep, and not smoking may help you prevent diabetes or manage your diabetes ABCs.
You don’t have to do it all at once. Start slow and build healthier habits from there.

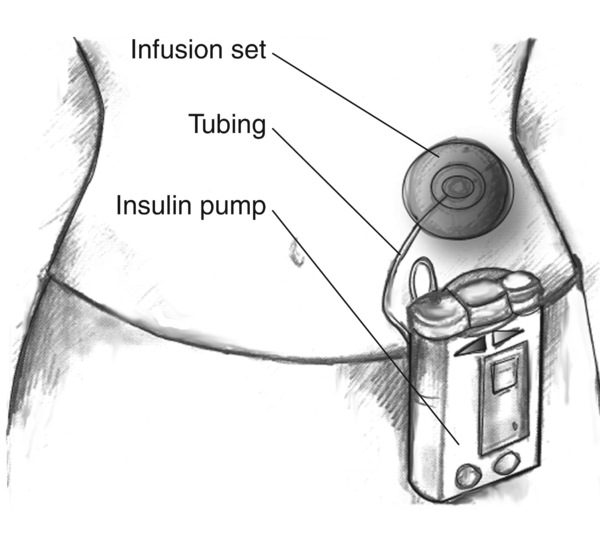
Using Diabetes Medications
Remember to take your medicines even if you feel healthy. Talk with your doctor or pharmacist if you have trouble taking your medicines on time or at the correct dose.
If you have trouble paying for medication, your doctor may suggest less costly alternatives.
Weight and Diabetes
If you have overweight or obesity, ask your primary care provider if healthy eating, physical activity, or other weight-loss treatments may help you manage your weight.

You may prevent or delay diabetes by losing 5 to 7 percent of your starting weight. Use the Diabetes Risk Management Calculator to determine how much weight you can lose to help reduce your risk of developing type 2 diabetes.
Manage Stress and Emotions
Managing diabetes can be hard. If you feel down, sad, or overwhelmed, learn about healthy ways to cope with stress. Consider talking to a mental health counselor or joining a support group.
Work with your Healthcare Team.
Managing diabetes takes a team. Your health care team may include a primary care provider, diabetes specialist, registered dietitian, or certified diabetes educator.
Ask your primary care provider if you should talk with other health care professionals about preventing or managing diabetes. These might include specialists for
- feet-podiatrists,
- skin-dermatologists,
- heart-cardiologists,
- eyes-opthalmologists.
Diabetes medicines, devices, and office visits can be expensive. A social worker or a member of your health care team may be able to help you find community resources or financial help for diabetes care.
Your health insurance provider may offer additional services to manage diabetes. Some employers offer preventive medicine services to their employees and their dependents.
Post Images and Graphics
The images and graphics are public use from the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health. I drew most of the content from the NIKKD website and added my insights.
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), is part of the National Institutes of Health. NIDDK research creates knowledge about and treatments for diseases that are among the most chronic, costly, and consequential for patients, their families, and the Nation.
The cover image of this post was created by JetPackAI available with WordPress.
Awareness and Action
There is much more to know about diabetes but the main point I hope you take away from this post is the importance of getting screened for diabetes. Take this short test to assess your risk.
Assess Your Risk
What was your score? Mine was 5 out of 10, that’s considered high risk. I knew that because my father had diabetes and developed heart disease as a result. I lost him to his disease many years ago. I wish his diabetes had been discovered sooner and that he had done more to keep it well controlled.
Once you are screened, ask your health care provider how often it should be repeated. There is no one right answer, it depends largely on your risk factors. Anytime you feel seriously ill, especially if you have any of the symptoms of diabetes, you should be tested again.
Testing for diabetes is a simple blood test, relatively inexpensive, so there is no reason not to test adults. Children and teenagers need testing less often, unless there are significant risk factors.
Learn more about diabetes signs in this post
10 Silent Signs of Diabetes
Diabetes mellitus type 2, often linked to obesity, complicates blood glucose control for overweight individuals. It contributes to serious complications such as heart disease, kidney failure, and neuropathy. Early diagnosis and effective management through lifestyle changes and medication are crucial. Everyone should be aware of symptoms and high-risk factors for diabetes.
Exploring the HEART of Health
I’d love for you to follow this blog. I share information and inspiration to help you transform challenges into opportunities for learning and growth.
Add your name to the subscribe box to be notified of new posts by email. Click the link to read the post and browse other content. It’s that simple. No spam.
I enjoy seeing who is new to Watercress Words. When you subscribe, I will visit your blog or website. Thanks and see you next time.
Use this search box for related posts on this blog or other topics of interest to you.