This information is current as of the date of original publication or update. It may have changed by the time you read this. I invite you to fact-check what you read here.
Please do not use this information for diagnosis or treatment purposes. Before making health decisions, discuss with your physician or other qualified healthcare provider.
I’m sharing this article originally published on KFF Health News. I have added hyperlinks for additional context. I have also added additional information for context, these are indicated in italics
As US Is Poised To Lose Measles-Free Status, RFK Jr.’s New CDC Deputy Downplays Its Significance
By Amy Maxmen January 21, 2026
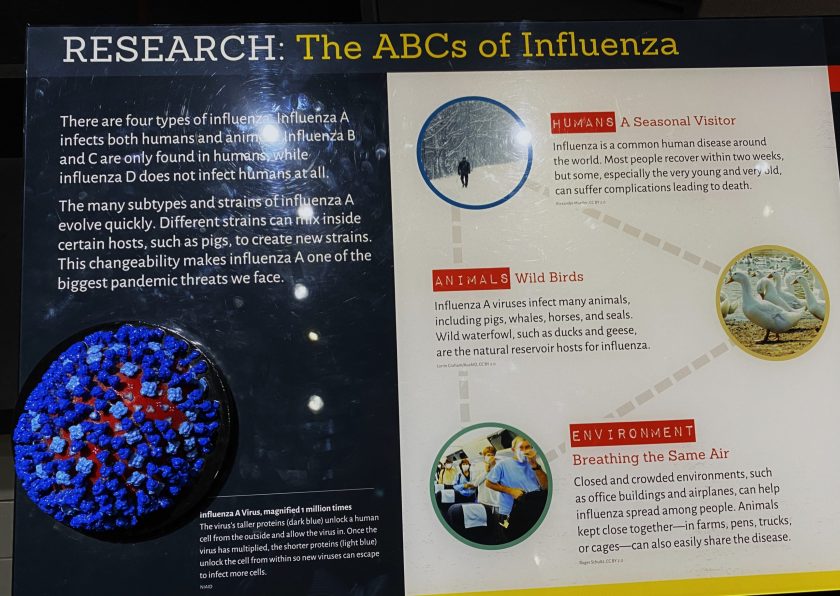
After a year of ongoing measles outbreaks that have sickened more than 2,400 people, the United States is poised to lose its status as a measles-free country.
However, the newly appointed principal deputy director at the Centers for Disease Control and Prevention, Dr. Ralph Abraham, said he was unbothered by the prospect at a briefing for journalists this week.
Before entering public office, Abraham practiced medicine and veterinary medicine for decades. He represented Louisiana in Congress from 2014 to 2020 and was appointed surgeon general of Louisiana last year.
“It’s just the cost of doing business with our borders being somewhat porous for global and international travel,” Dr. Abraham said. “We have these communities that choose to be unvaccinated. That’s their personal freedom.”
Infection from Abroad vs. Domestic
Infections from other countries, however, accounted for only about 10% of measles cases detected since Jan. 20, 2025, the official start of the deadly measles outbreak in West Texas, which spread to other states and Mexico. The rest were acquired domestically.
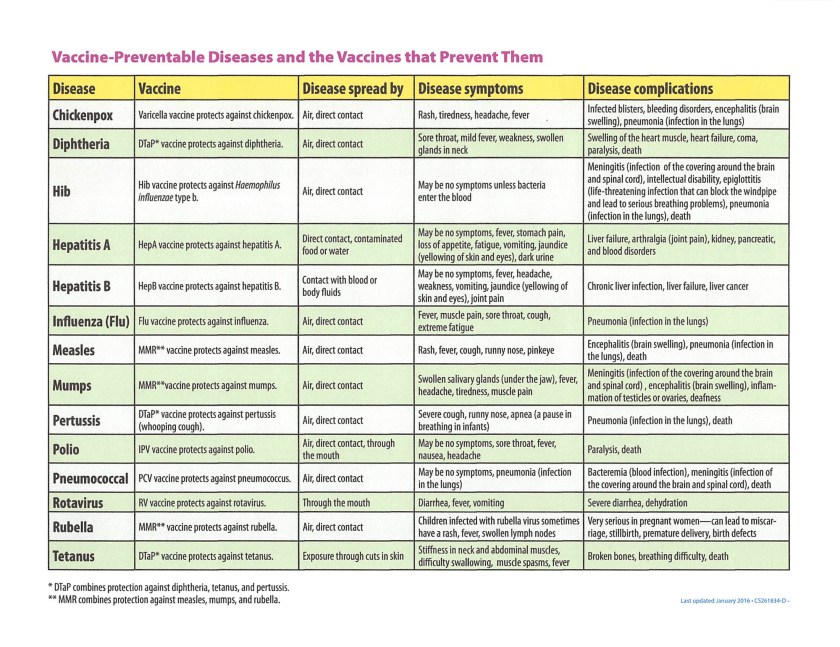
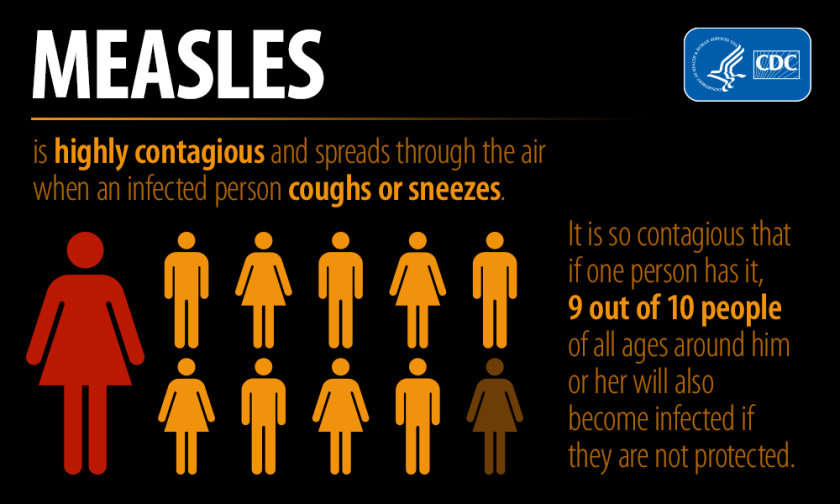
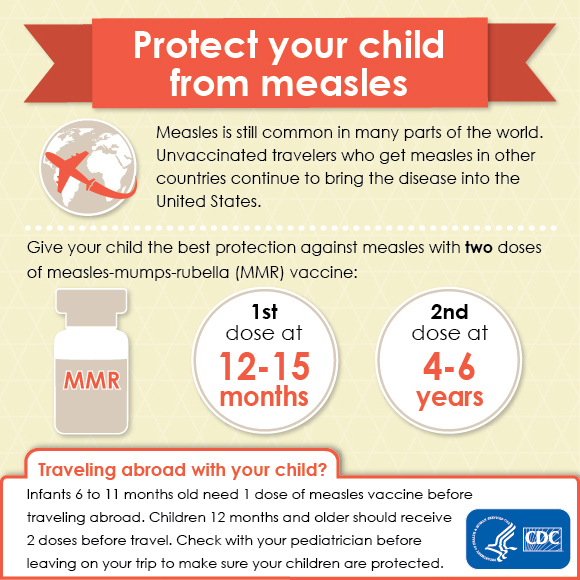
This marks a change since the U.S. eliminated measles in 2000. Measles occasionally popped up in the U.S. from people infected abroad, but the cases rarely sparked outbreaks, because of extremely high rates of vaccination. Two doses of the measles, mumps, and rubella vaccine strongly prevent infection and halt the virus’s spread.
Measles DNA detectives
To maintain its measles elimination status, the U.S. must prove that the virus has not circulated continuously in the nation for a year, between Jan. 20, 2025, and Jan. 20, 2026. To answer the question, scientists are examining whether the major outbreaks in South Carolina, Utah, Arizona, and Texas were linked.
Health officials confirmed that the main measles virus strain in each of these outbreaks is D8-9171. But because this strain also occurs in Canada and Mexico, CDC scientists are now analyzing the entire genomes of measles viruses — about 16,000 genetic letters long — to see whether those in the United States are more closely related to one another than to those in other countries.
The CDC expects to complete its studies within a couple of months and make the data public. Then the Pan American Health Organization, which oversees the Americas in partnership with the World Health Organization, will decide whether the U.S. will lose its measles elimination status. And that would mean that costly, potentially deadly, and preventable measles outbreaks could become common again.
(However, the United States has withdrawn from the World Health Organization.)
Reponse from Infection Experts
“When you hear somebody like Abraham say ‘the cost of doing business,’ how can you be more callous,” said pediatrician and vaccine specialist Paul Offit, in an online discussion hosted by the health blog Inside Medicine on Jan. 20, 2026.
Dr. Offit is the Director of the Vaccine Education Center and an attending physician in the Division of Infectious Diseases at Children’s Hospital of Philadelphia, as well as a Professor of Pediatrics at the University of Pennsylvania School of Medicine.
“Three people died of measles last year in this country,” Dr. Offit added. “We eliminated this virus in the year 2000 — eliminated it. Eliminated circulation of the most contagious human infection. That was something to be proud of.”
Jennifer Nuzzo, director of the Pandemic Center at Brown University, disparaged the Trump administration’s focus on finding genetic technicalities that may spare the country’s measles-free status. “This is the wrong thing to pay attention to. Our attention has to be on stopping the outbreaks,” she said.
“If we keep our status, it should be because we have stopped the spread of measles,” she said. “It’s like they’re trying to be graded on a curve.”
Jennifer Nuzzo is a nationally and globally recognized leader on global health security, public health preparedness and response, and health systems resilience.
HHS and CDC Vaccine Policy Shifts
Dr. Abraham said vaccination remains the most effective way to prevent measles but that parents must have the freedom to decide whether to vaccinate their children. Several states have loosened school vaccine requirements since 2020, and vaccine rates have dropped. A record rate of kindergartners, representing about 138,000 children, obtained vaccine exemptions for the 2024-25 school year.
Information on vaccines has been muddied by Health and Human Services Secretary Robert F. Kennedy Jr., who previously founded an anti-vaccine organization. He has undermined vaccines throughout his tenure. On national television, he has repeated scientifically debunked rumors that vaccines may cause autism, brain swelling, and death.
The Trump administration impeded the CDC’s ability to assist West Texas during the first critical weeks of its outbreak and slowed the release of federal emergency funds, according to KFF Health News investigations.
However, the agency stepped up its activity last year, providing local health departments with measles vaccines, communication materials, and testing. Dr. Abraham said HHS would give South Carolina $1.5 million to respond to its outbreak, which began nearly four months ago and had reached 646 cases as of Jan. 20.
If the CDC’s genomic analyses show that last year’s outbreaks resulted from separate introductions from abroad, political appointees will probably credit Kennedy for saving the country’s status, said Demetre Daskalakis, a former director of the CDC’s national immunization center, who resigned in protest of Kennedy’s actions in August.
And if studies suggest the outbreaks are linked, Daskalakis predicted, the administration will cast doubt on the findings and downplay the reversal of the country’s status: “They’ll say, who cares.”
Indeed, at the briefing, Dr. Abraham told a reporter from Stat that a reversal in the nation’s status would not be significant: “Losing elimination status does not mean that the measles would be widespread.”
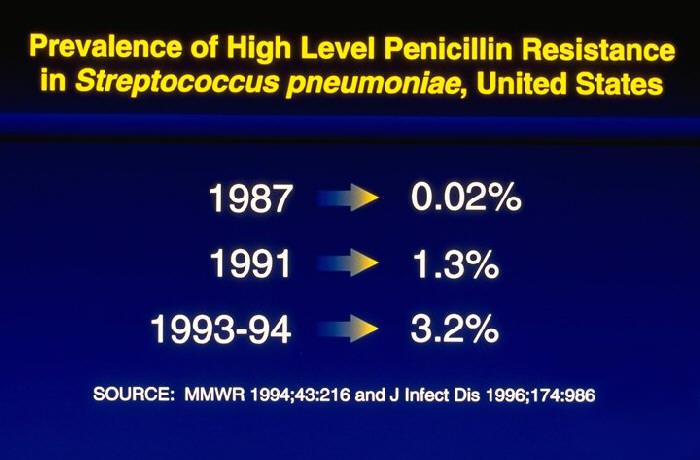
Data shows otherwise. Case counts last year were the highest since 1991, before the government enacted vaccine policies to ensure that all children could be protected with measles immunization.
Lauren Sausser contributed reporting.
Amy Maxmen, KFF Health News public health local editor and correspondent, covers efforts to prevent disease and improve well-being outside of the medical system, and the obstacles that stand in the way. Before joining KFF Health News in 2024, she was a senior reporter at Nature covering health inequities, global health, infectious diseases, and genomics. She earned a Ph.D. from Harvard University in evolutionary biology.
This story also ran on Healthbeat. It can be republished for free.
Oklahoma Voice shared this story.
Measles, Mumps, Rubella Vaccination Recommendation Summary
Images in this Post
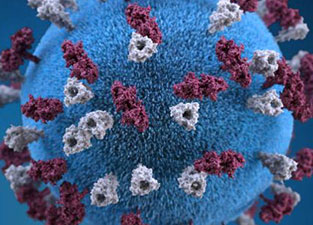
The cover illustration is a 3D graphic representation of a spherical-shaped, measles virus particle, that was studded with glycoprotein tubercles. Those tubercular studs colorized maroon, are known as H-proteins (hemagglutinin), while those colorized gray, represented what are referred to as F-proteins (fusion).
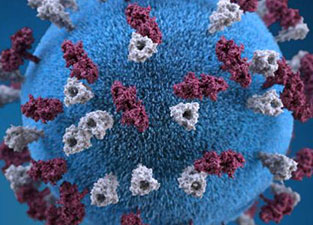
The F-protein is responsible for fusion of the virus and host cell membranes, viral penetration, and hemolysis. The H-protein is responsible for the binding of virions to cells. Both types of proteinaceous studs are embedded in the particle envelope’s lipid bilayer.
Illustrator: Alissa Eckert, Content provider:CDC/ Allison M. Maiuri, MPH, CHES, Public Domain
Exploring the HEART of Health
I’d love for you to follow this blog. I share information and inspiration to help you transform challenges into opportunities for learning and growth.
Add your name to the subscribe box to be notified of new posts by email. Click the link to read the post and browse other content. It’s that simple. No spam.
I enjoy seeing who is new to Watercress Words. When you subscribe, I will visit your blog or website. Thanks and see you next time.
Use this search box for related posts on this blog or other topics of interest to you.