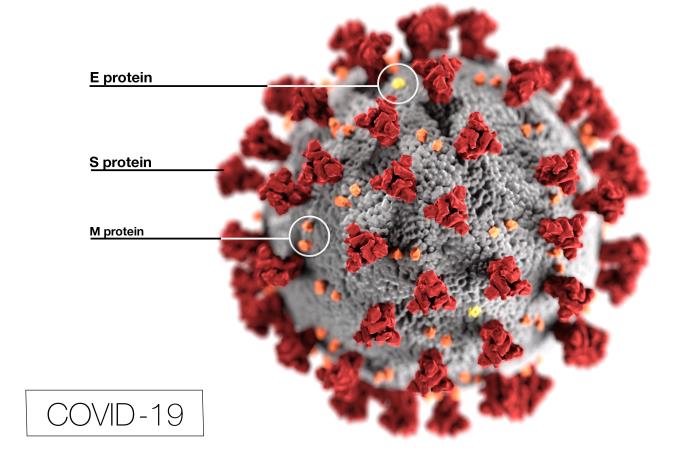
” In a very short period, health care and society have been severely challenged by yet another emerging virus. Preventing transmission and slowing the rate of new infections are the primary goals.
However, the concern of COVID-19 causing critical illness and death is at the core of public anxiety.”
JAMA, March 11, 2020 “Care for Critically Ill Patients with COVID-19”
“just a virus”
You’ve probably visited your doctor or your child’s doctor for an acute illness that started suddenly or over a few days. Likely the symptoms included some combination of
- fever and/or chills
- sore throat, runny nose, and/or sneezing
- cough
- joint and/or muscle aches
- vomiting with or without diarrhea
- rash
- redness with or without drainage from the eyes
- headache and a general miserable feeling
And you were probably told that you or your child had “a virus”,or viral infection, followed by one or more of the following phrases-
- there is no treatment but it will go away
- the treatment will not cure it, but it will help the symptoms
- it has to run it’s course
- it resolves without treatment
- you caught it from someone else
- it is contagious
- the symptoms will go away, but it stays in your body
- you may get it again
- you won’t get it again
- there is a vaccine to prevent this
- there is no vaccine to prevent this
And finally, you may have heard a phrase I hope you never hear, and I hope we doctors never use again-
“It’s JUST a virus.”
Why it’s never “just a virus”
The quote at the beginning of this post is from an article in the Journal of the AMA . Unless you haven’t listened to any news for the past 8 weeks, you are well aware of the “challenge” the whole world has been confronting over what some do call “just a virus”; and you know that it has caused much critical illness and death, leading to “public” and private anxiety.
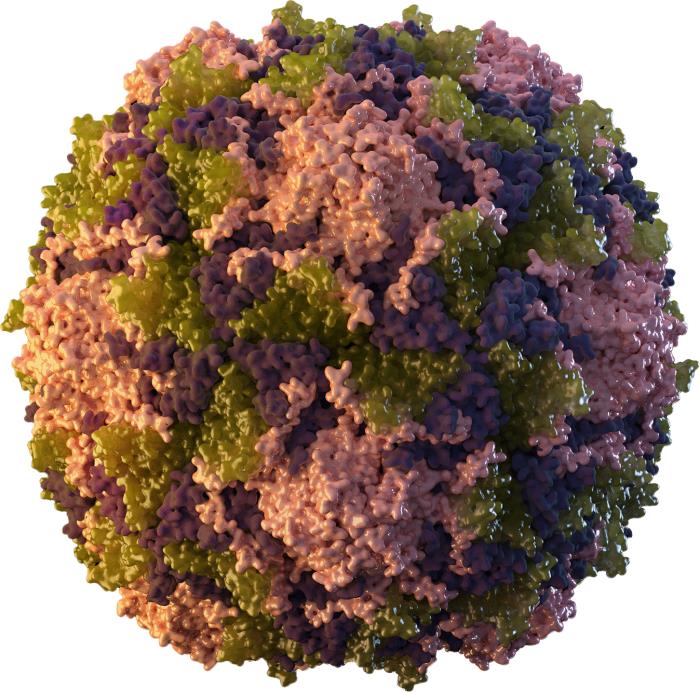
But we shouldn’t have been surprised. Viruses have been around probably as long as humans have, we just didn’t know much about them until the past century or so. After all, viruses are made of genetic material DNA or RNA, like us and animals; when viral DNA/RNA invades our bodies and enters our cells, they start reproducing (replicating), causing disease. (This is a simplified explanation of what viruses do.)
How do doctors know it’s a virus?
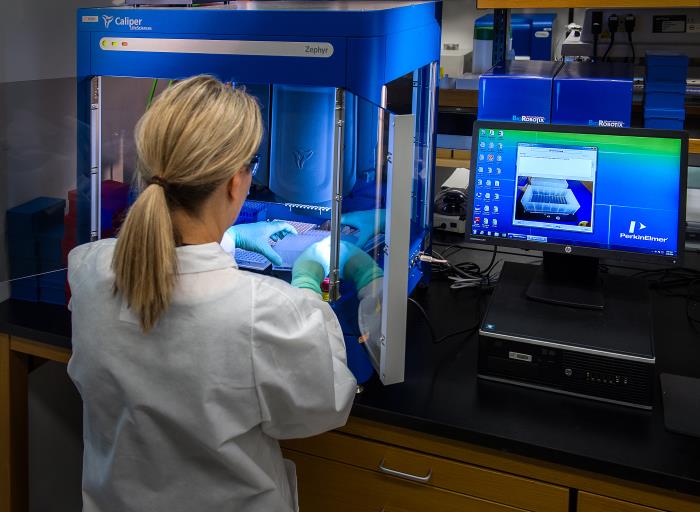
Until fairly recently, viral infections were diagnosed by typical symptoms and characteristic physical exam findings, especially fever and rash, and many are still diagnosed that way. Then laboratory scientists developed tests for some viruses, which help confirm the diagnosis , important when a treatment is available. The tests can also be used to know if someone is or is not already immune to a disease, if a vaccine is available.
So what infections are caused by viruses?
Lots of them are, but fortunately most are not nearly as serious as the novel coronavirus that causes COVID-19, or the 2 previous coronavirus outbreaks, SARS and MERS. You’re probably quite familiar with some of them. Here’s what I think is an easy to understand way to categorize them.
categories of viral infections
This is how they behave without previous vaccination or treatment (when available) .This is not an exhaustive list, just some of the most common. These all spread person to person.
Short duration, followed by life-long immunity
- measles
- mumps
- rubella
- polio
- hepatitis A
Short duration, followed by short-lived immunity
- RSV- respiratory syncytial virus
- influenza
- rhinovirus (common cold)
- coronavirus
Persistent infection, life-long carrier of virus, virus inactive at times, not always passed to other people
- HSV-herpes simplex virus
- VZ-varicella/zoster (chicken pox-shingles)
Persistent infection, life-long carrier of virus, virus always active and can be passed to other people
- HIV/AIDS-human immunodeficiency virus
- Hepatitis B
- Hepatitis C
- HPV-human papilloma virus
Viruses that spread from animals to humans
- Avian influenza
- Rabies
- West Nile virus
Viruses that spread from animals to humans-and sometimes then to other humans
- yellow fever
- coronavirus
- Ebola

How serious are viral infections?
How serious a viral infection is depends on how you want to define “serious”. Even a “mild” illness can be a major problem if it’s you or your family that is sick. With a mild illness, you still may feel too sick to work or go to school, which you should not do anyway, so not to transmit it to other people.
The above classification is quite simplified, a framework for looking at infections that you’ve probably heard of. They range from the common cold, with no risk of death, to HIV/AIDS and rabies, which are always fatal without treatment.
People with the short duration infections usually recover but some carry risk of progressing into life threatening respiratory events, due to RSV, influenza, and now the coronaviruses. Polio frequently left its victims paralyzed for life and measles can cause permanent deafness.
The herpes virus and VZ virus cause recurrent outbreaks of painful skin sores. . Hepatitis B and C viruses can lead to chronic liver disease and liver cancer. HPV causes benign warts but also cancer of the cervix.
“the challenge of emerging virus”
I hope that we all learn from this pandemic. I hope both physicians and patients take viral infections more seriously and appreciate the complexity and challenge they represent. We share something important with them-DNA, the genetic material that creates health as well as disease. Viruses aren’t static; like us they change and adapt.
We have vaccines that can dramatically reduce our risk of getting several of these diseases and I hope more people will use them. We have a few drugs which combat these diseases; fortunately some have been life saving, like those for HIV/AIDs.
Healthy lifestyles offer protection against infections of all kinds but we frequently overlook their value. You may be tired of hearing them but they include
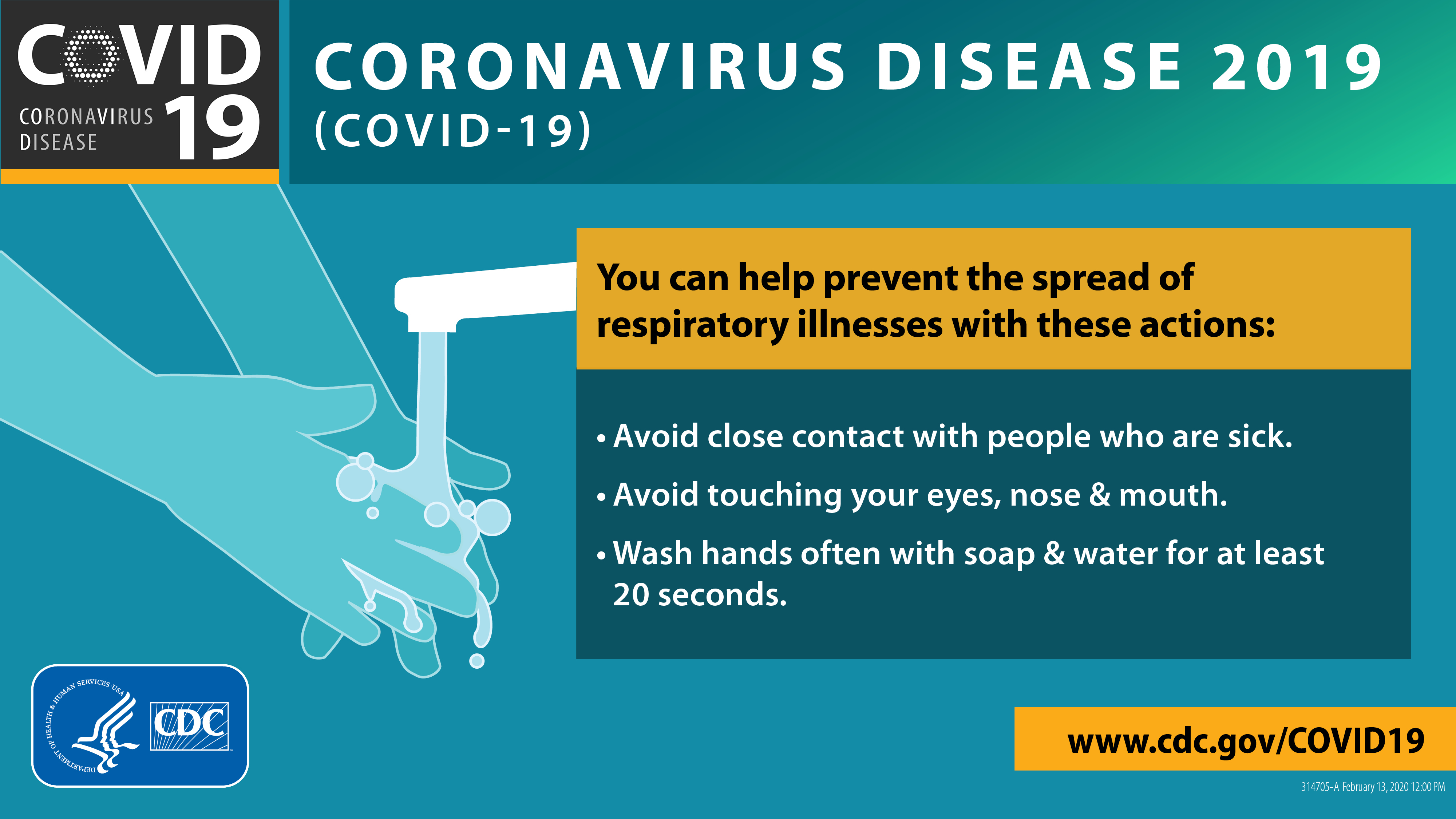
- hand washing- often and thoroughly
- cleaning and disinfecting frequently touched surfaces
- water and sanitation facilities
- safe food handling and cooking practices
- wise sexual practices
- staying home when sick
- limiting contact with animals and preventing insect bites
- immunization
sharing the HEART of health
For this post I reviewed sections of the textbook Fenner and White’s Medical Virology, Fifth Edition , made available online free at ScienceDirect.com specifically to help medical professionals navigate the COVID-19 challenge.
You might want to check out some less technical references at these links.
Overview of Viral Infections
Viral Infection
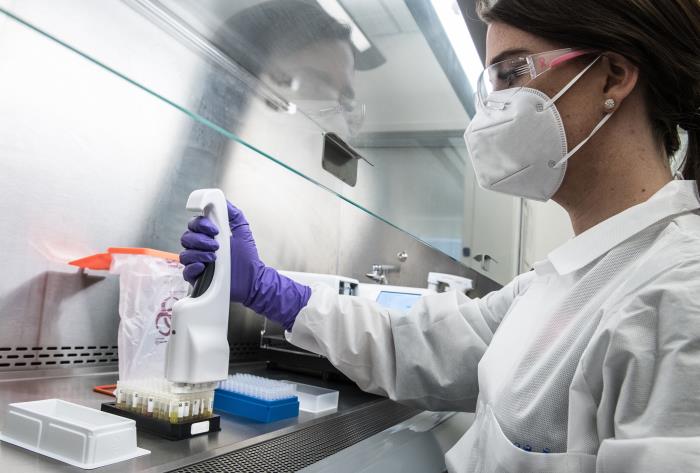
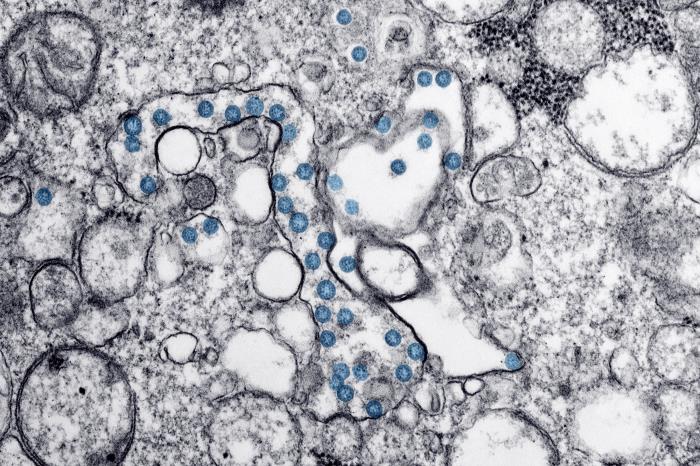
Except for the cover photo, the pictures in the post are from the Centers for Disease Control and Prevention website, and are in the public domain.