updated November 26, 2024
I originally wrote this post in 2020 during the Presidential campaign between incumbent Donald Trump, Republican, and Joe Biden, Democrat. Trump was not reelected.
In 2024 Trump again ran for President against the incumbent Biden, who unexpectedly dropped out of the race in the summer. His Vice President Kamala Harris became the Democratic candidate.
Donald Trump won reelection with 50% of the popular votes to 48.4% for Kamala Harris. The electoral count was 312 to 226. (per the Associated Press).
Healthcare in a Pandemic-2020
The year 2020 looked to be historic even prior to the coronavirus pandemic, police involved shootings, riots, and Black Lives Matter protests. The USA will choose the next president, impacting the economy, security, defense, education, and healthcare.
As President, Mr. Trump heads the Executive Branch of the U.S. Government.
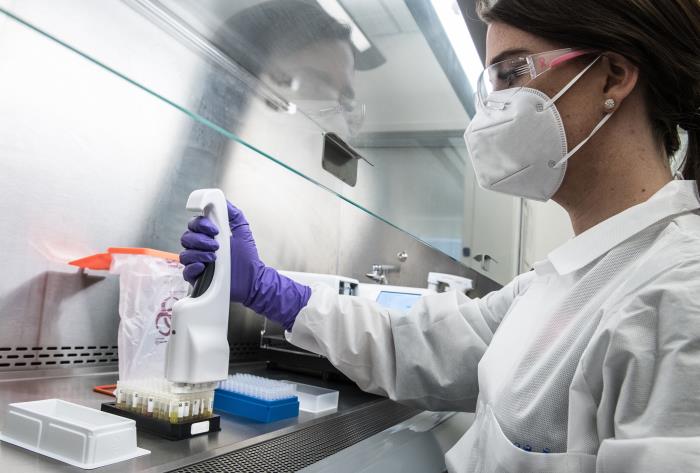
The Department of Health and Human Services, headed by Cabinet Member Alex Azar manages the response to COVID-19. Other Cabinet members and their Departments are involved as well.
The agencies most involved in the COVID-19 response include
- Health and Human Services-HHS
- Federal Emergency Management Agency-FEMA
- Centers for Disease Control-CDC
- National Institutes of Health-NIH
- Federal Drug Administration-FDA
- Small Business Administration-SBA
- Veterans Administration-VA
- Department of Defense -DOD
- Treasury Department
- State Department
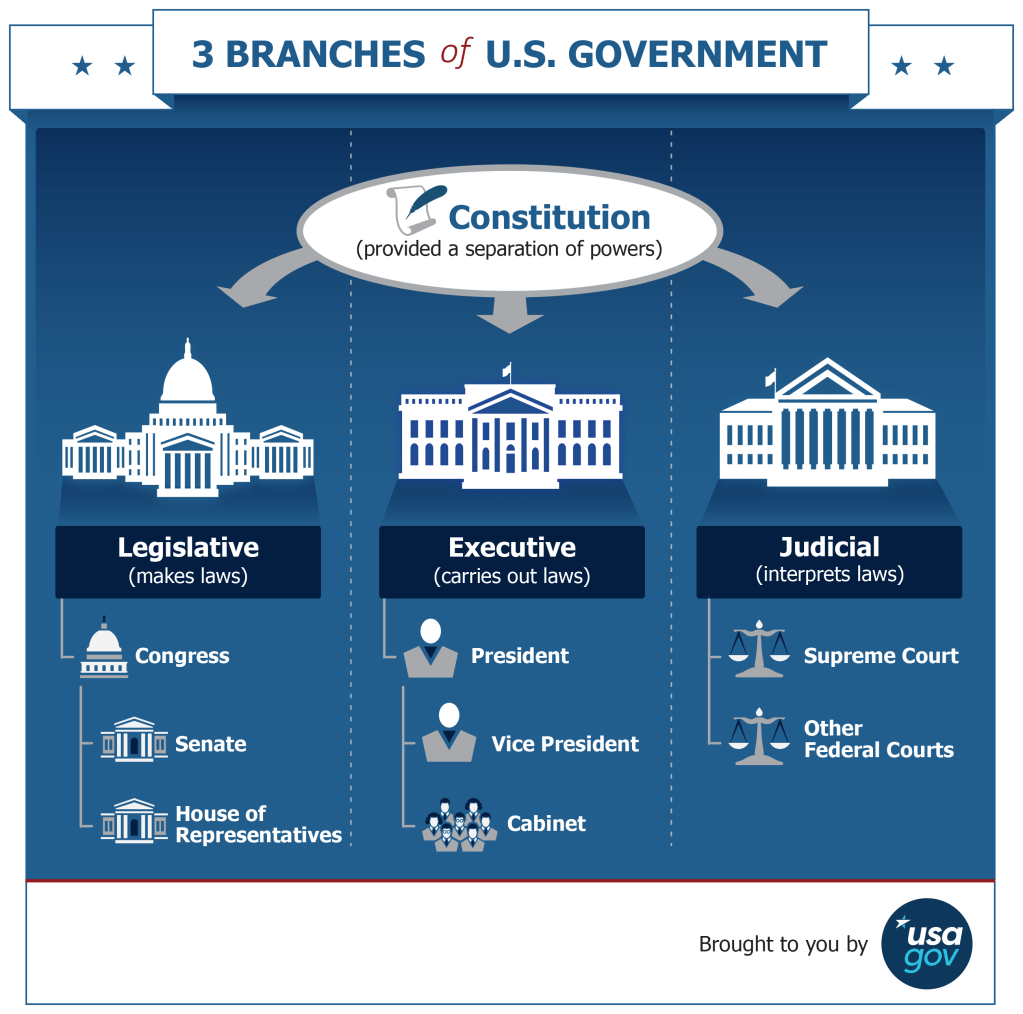
President Trump established a Coronavirus Task Force which advises him on the medical and scientific facts, research, and treatment of COVID-19.Vice President Mike Pence chairs the task force.
In this review I’m highlighting Mr. Trump’s statements and actions, not those attributed to his “Administration”.
TIMELINE: THE TRUMP ADMINISTRATION’S DECISIVE ACTIONS TO COMBAT THE CORONAVIRUS
The following was adapted from a link that is no longer active
While Democrats play politics, the Trump Administration is working tirelessly to combat the coronavirus and provide economic relief to affected Americans:
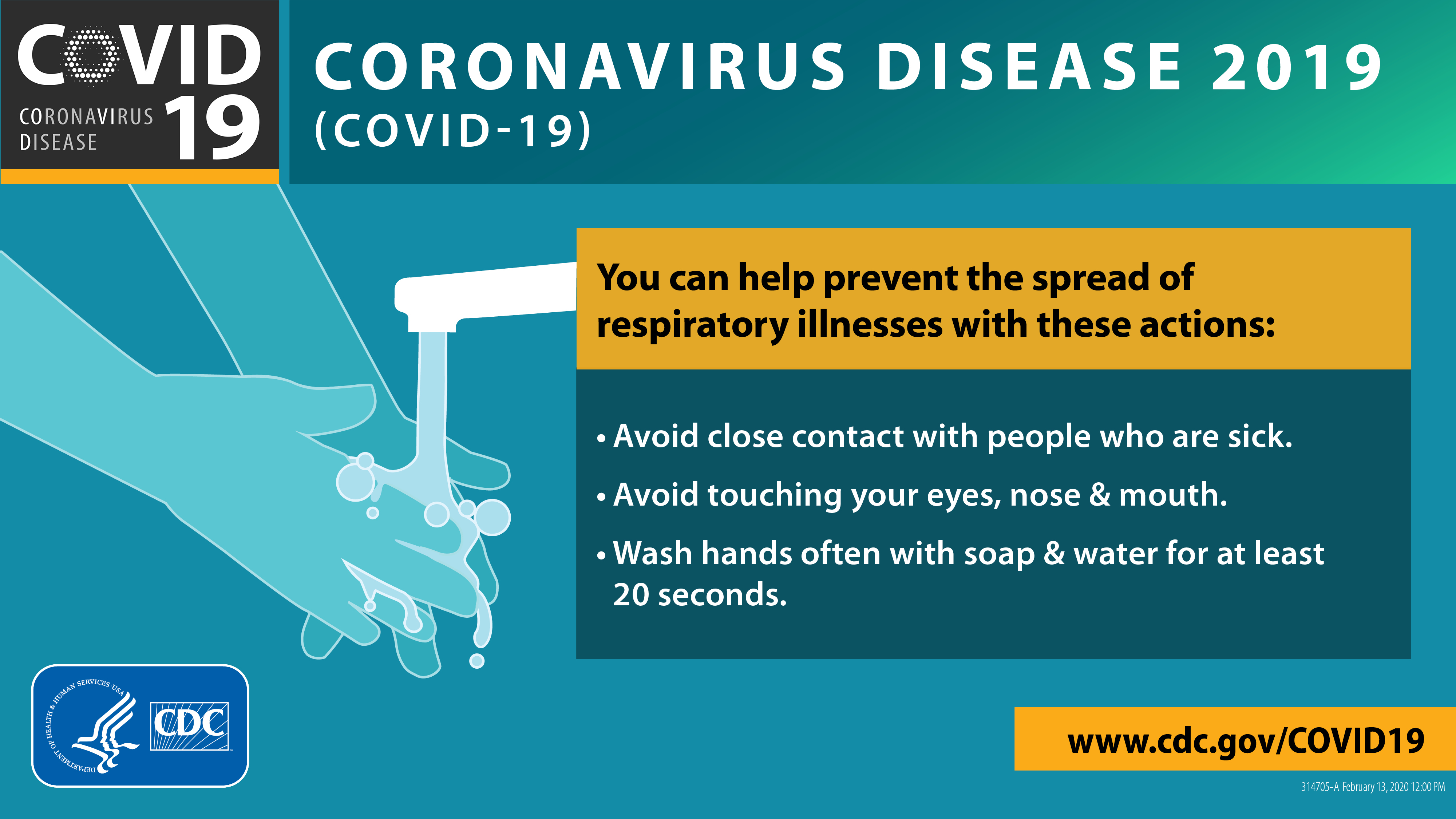
President Trump is taking concrete actions to rapidly expand testing and guarantee any American can get tested for coronavirus for free
President Trump is taking decisive action to make sure U.S hospitals have the resources they need to mobilize against the coronavirus.
President Trump is taking critical steps to shore up the U.S. economy and help Americans economically impacted by the coronavirus.
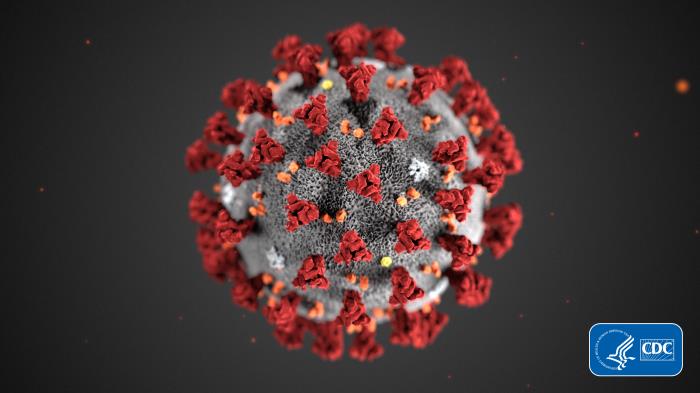
December 31, 2019-China reports the coronavirus to WHO-the World Health Organization.
January 6, 2020- the CDC issued a level 1 travel notice for Wuhan China, established a coronavirus incident management system for information about the virus, and two weeks later activated its emergency operations center.
January 27- The White House Coronavirus Task Force started meeting to monitor the virus and provide updates to the President. The CDC issued a level lll travel health notice to avoid all nonessential travel to China.
January 30-WHO declared coronavirus disease 2019, COVID-19, a global health emergency. (not in the timeline as written)
On January 31, the Trump Administration declared the coronavirus a public health emergency, announced Chinese travel restrictions, and suspended entry into the United States for foreign nationals who pose a risk of transmitting the coronavirus.
February 4- In his State of the Union Address, Mr Trump vowed to “take all necessary steps” to protect Americans from the coronavirus.
February 7- He told reporters that the CDC is working with China on the coronavirus.
February 24- The Trump Administration requested $2.5 billion from Congress to combat the coronavirus spread. On March 6 he signed an $48.3 billion bill to provide funds to federal, state, and local agencies, and $500 million in Medicare telehealth waivers. He requested a payroll tax cut bill from Congress.
He also
- Requested low interest small business loans by the SBA
- Deferred tax payments to the Treasury Department
- Signed the Families First Coronavirus Response Act for free testing and paid sick leave
- Moved tax day from April 15 to July 15
- Signed the Coronavirus Aid, Relief, and Economic Security-CARES-Act
March 31- Trump issued “30 Days To Slow The Spread” guidance to mitigate the outbreak of coronavirus.
April 2-Mr. Trump invoked the Defense Production Act to direct 3M to produce more N95 respirator masks and to help several companies-ResMed, General Electric, Medtronic- get the supplies needed to make ventilators.
April 3-Mr. Trump signed a Presidential Memorandum blocking the export of N95 and other respirator masks, surgical masks, PPE gloves, and surgical gloves to ensure they are available in the U.S.; he directed FEMA to send Ochsner ( Medical Center in Louisiana) surgical gowns.
April 6- In a phone call, he discussed potential coronavirus therapies with CEOs of pharmaceutical and biotech companies.
April 12- The United States, Russia, and OPEC agreed to cut oil production and stabilize the oil market, a deal that Mr.Trump “brokered.”
April 14-President Trump halted funding to WHO, while a review of its “mismanagement” of the coronavirus outbreak is conducted. (quotation marks added)
April 16-He announced new, phased “opening up America again” guidelines, spoke with the Opening Up America Again Congressional group, and spoke with the Governors about re-opening.
By April 17, the President had declared major disaster declarations for all states and territories, a first in U.S. history
April 22- Mr. Trump signed a Presidential Proclamation suspending immigration to the U.S. for 60 days due to “the impact of foreign workers on the labor market, in an environment of high unemployment.”
By April 27, President Trump had spoken with many foreign leaders, including those of India, Italy, China, Turkey, Russia, Kenya, South Africa, Poland, Pakistan, Qatar, Ecuador, Britain, and France.
He also spoke to Republican Senators, former Vice President Joe Biden, and the state Governors.
He attended meetings with multiple business leaders including those in health insurance, tourism, retail, wholesale, supply chain distributors,and banking.
He spoke by phone with owners of groceries, restaurants, and other small businesses.
He also spoke to leaders in mental health, faith, tribal affairs, and nonprofits, including the Salvation Army and the Red Cross.
He met with energy execs from Phillis 66, Devon, Occidental, Chevron, Exxon Mobil, and other companies to discuss coronavirus’ effect on the energy industry.
Mr. Trump spoke to the commissioners of major league sports organizations-MLB, NFL, and NBA, recognizing the teams’ and players’ work in their communities to combat coronavirus.
He met with military families, coronavirus survivors, and front line healthcare workers.
April 24- The President signed the Paycheck Protection Program ( PPP) and Health Care Enhancement Act into law
- $323 billion-for the PPP
- $75 billion-for health care providers
- $25 billion- for coronavirus testing
April 24-President Trump spoke with three other Presidents.
April 24: “Vice President Pence & members of the coronavirus held a conference call with Governors to discuss increasing testing capacity.”
On April 27, the White House coronavirus task force appeared in a Rose Garden event. The topic: “Opening Up America Again.” (from a report by CNBC)
Exploring the HEART of health
I’d love for you to follow this blog. I share information and inspiration to help you transform challenges into opportunities for learning and growth.
Add your name to the subscribe box to be notified of new posts by email. Click the link to read the post and browse other content. It’s that simple. No spam.
I enjoy seeing who is new to Watercress Words. When you subscribe, I will visit your blog or website. Thanks and see you next time.