look for an updated version of this post on July 2, 2021
In ophthalmology, visual acuity is measured by the distance one can see compared to “normal”. 20/80 vision means at 20 feet you only see what a normal vision person can see from 80 feet. Perfect vision is labeled 20/20.
Maybe you expected 2020 to be a perfect year. I didn’t expect perfection, but I hoped it would be better than last year, when my husband and I spent 8 months mostly homebound while he recovered from a devastating ankle fracture.
But instead this year has brought
- a contentious presidential election and an unexpected serious pandemic
- peaceful protests and raucous riots
- racism confrontations and reconciliation pursuits
- health inequities battles and healthy community pursuits

Independence Day 2020
Every year on July 4th the United States celebrates Independence Day- the day in 1776 the original 13 American colonies established an independent country.
A few years later they established a government as specified in the Constitution of the United States, to “form a more perfect Union”.
The United States Constitution
The Constitution does not specifically mention, establish, create, or endorse a healthcare system. Some phrases in the Preamble hint at it though-
- establish Justice
- insure domestic Tranquility
- provide for the common defense
- promote the general Welfare
Government sponsored health care programs
The Affordable Care Act, aka Obamacare
The United States Congress passed the Patient Protection and Affordable Care Act (ACA) in 2010 to guarantee basic health insurance to all citizens. During the last presidential campaign, President Trump vowed to “repeal and replace” this law but although it has been modified, it is still in place.
Healthcare for military service members, veterans ,and their families
During the American Revolution the fledgling government extended health care benefits to the soldiers and veterans of that war; that system evolved into the current Department of Defense military health care system which covers service members and the Veterans’ Administration system for veterans.
Medicare and Medicaid
Two other government healthcare programs- Medicare and Medicaid are over 50 years old.
Medicaid provides insurance coverage for adults and children who are unemployed or low income.
Medicare covers disabled children and adults and persons 65 years and older.

Department of Health and Human Services
Most of the health care activities of the federal government fall under the agencies of the Department of Health and Human Services or HHS. The Secretary of HHS serves in the President’s Cabinet.
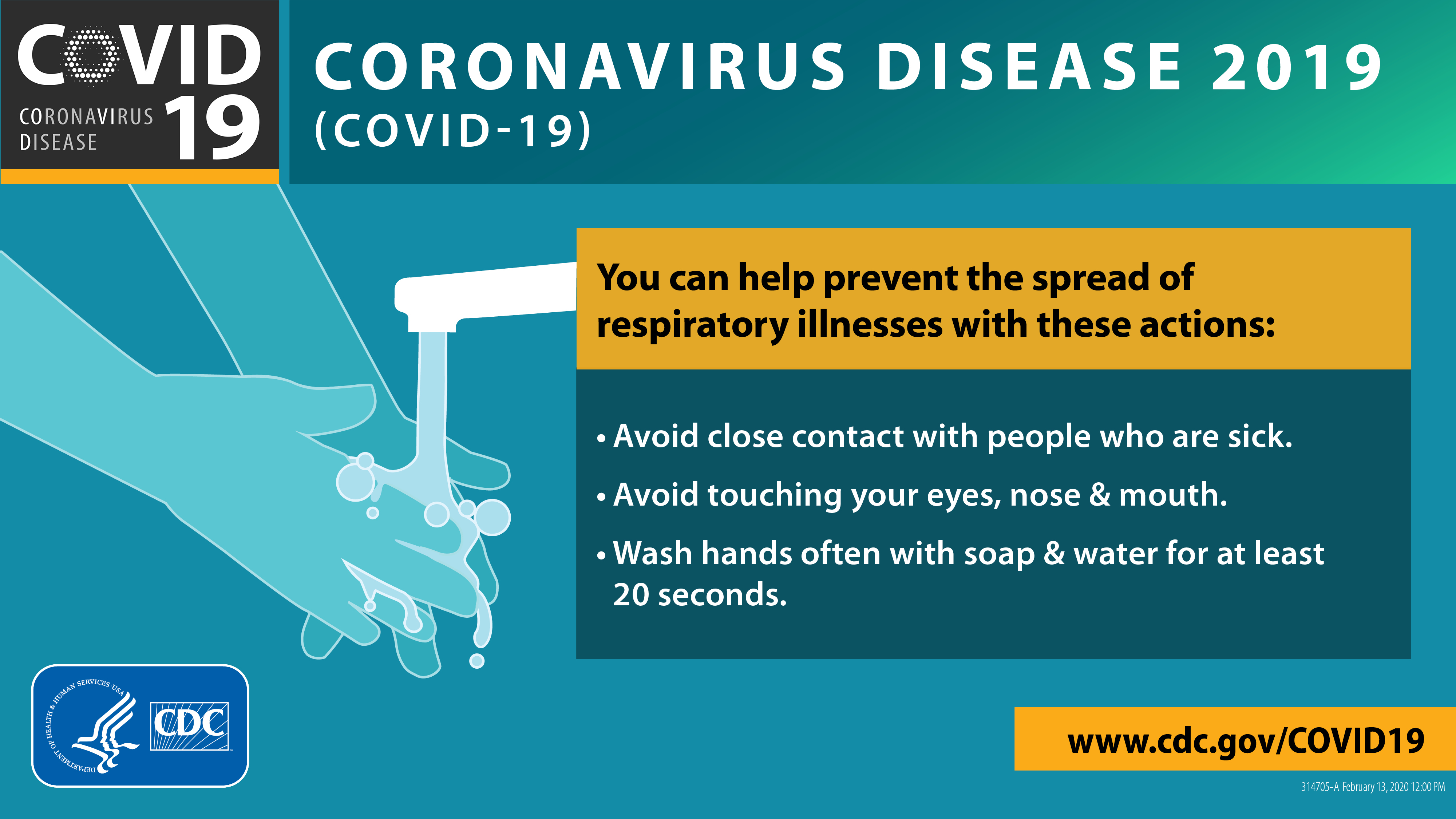
Due to the COVID-19 pandemic, we’ve heard more about the HHS in the news than usual; maybe you’ve never heard of these agencies. Generally, management of a pandemic or other public health emergency falls within the work of the CDC.
Centers for Disease Control and Prevention–
The CDC’s mission is simple but encompasses many facets of health
“to work 24/7 to protect America from health, safety and security threats, both foreign and in the U.S.”
The CDC website devotes an entire section now to information, guidelines, and news about the SARS-CoV-2 virus and COVID-19.

The goal of public health is to avoid or prevent health threats from becoming public health emergencies, like the COVID-19 pandemic. If they accomplish the mission, we hardly notice. But when an outbreak occurs, their work suddenly becomes visible, scrutinized, and debated.
The CDC director, Dr. Robert Redfield, spoke to Congress soon after the pandemic started, and his assessment of the response and funding for it were not positive. Lack of funding hampered the federal government’s response to the coronavirus outbreak, he told lawmakers on March 10, 2020.
“The truth is we’ve underinvested in the public health labs,There’s not enough equipment, there’s not enough people, there’s not enough internal capacity, there’s no search capacity”
Dr. Robert Redfield, Director, CDC
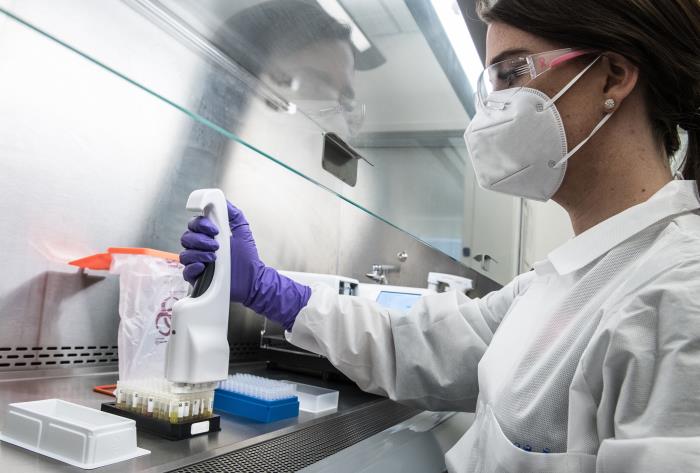
The Trump administration subsequently enlisted private companies to help cut the difference. The CDC partnered with Integrated DNA Technologies to manufacture the tests under a CDC contract. IDT partnered with commercial labs, including LabCorp and Quest, for the testing.
This was reported at CNBC. at the following link.
Coronavirus testing delays caused by lack of funding for public health labs
National Institutes of Health– NIH
The National Institutes of Health, part of the Public Health Service,
- supports biomedical and behavioral research with the United States and abroad,
- conducts research in its own laboratories and clinics,
- trains promising young researchers, and
- promotes collecting and sharing medical knowledge.
And within the NIH is the NIAID– the National Institutes of Allergy and Infectious Diseases, which has been an invaluable source of guidance as the United States and the world works to understand and manage this new infectious disease.
Strategic Plan for COVID-19 RESEARCH
- Improve fundamental knowledge of SARS-CoV-2 and COVID-19
- Support the development of diagnostics and assays
- Characterize and test therapeutics
- Develop safe and effective vaccines against SARS-Cov-2
Read the full report at the link.
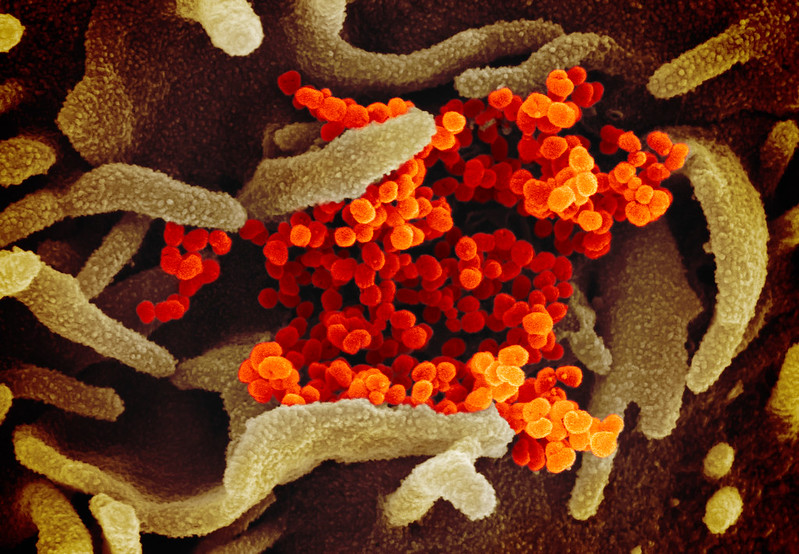
credit NIH, public domain
Credit: National Institute of Allergy and Infectious Diseases-Rocky Mountain Laboratories, NIH
Food and Drug Administration– FDA
The FDA joins the pandemic response by
- reviewing and approving diagnostic tests for the coronavirus
- protecting consumers from fraudulent products for COVID-19.
- issuing Emergency Use Authorizations (EUAs) for ventilators
- sampling and testing of respirators for importation
As of June 26 there are 153 currently authorized tests under EUAs; these include 129 molecular tests, 23 antibody tests, and 1 antigen test.
There are currently no FDA-approved products to prevent or treat COVID-19. Consumers concerned about COVID-19 should consult with their health care provider.
Occupational Safety and Health administration-OSHA
OSHA is part of the United States Department of Labor. OSHA’s administrator answers to the Secretary of Labor, who is a member of the cabinet of the President of the United States.
Congress created the Occupational Safety and Health Administration (OSHA) in 1970 to
ensure safe and healthful working conditions for working men and women by setting and enforcing standards and by providing training, outreach, education and assistance.
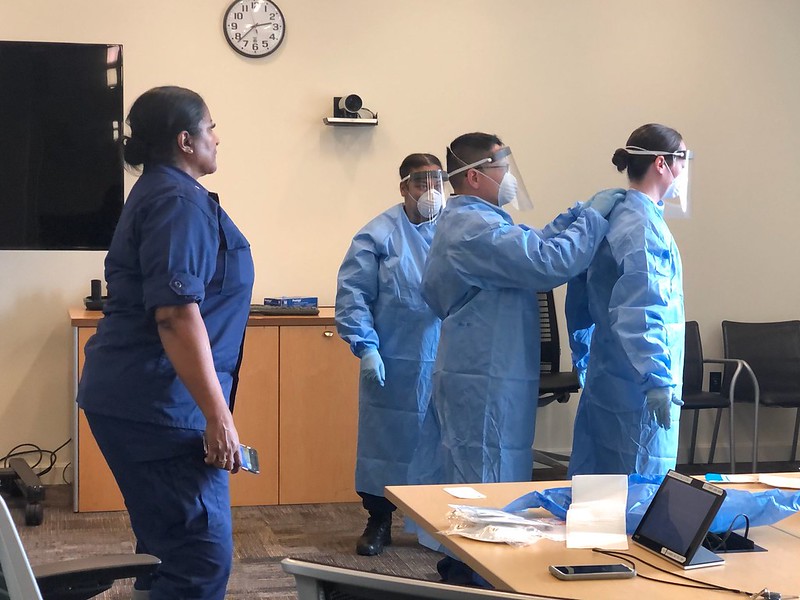
For the pandemic response, OSHA offers guidance on
- returning to work
- preparing workplaces for COVID-19
- worker exposure risk to COVID-19
- for specific industries including airlines, farms, retail, corrections
- use of respiratory protection equipment
This page on the OSHA website explains the
key differences between cloth face coverings, surgical masks, and respirators.
important laws that administer and regulate both private and public healthcare.
The Affordable Care Act- ACA
Health Insurance Portability and Accountability Act-HIPPA
Emergency Medical Treatment and Labor Act- EMTALA
Americans with Disabilities Act-ADA
Family Medical Leave Act-FMLA

Let Freedom Ring
In the Declaration of Independence, the founders of the United States created a nation based on the “self-evident truths” of “Life ,Liberty, and the pursuit of Happiness” and to promote “Safety and Happiness” .
They didn’t mention “healthcare” either, maybe because in the late 1700s medical practice was more superstition than science.
Surgery was rudimentary due to no anesthesia and infections frequently proved deadly due to no antibiotics.
No one had even imagined, much less identified the human genome, and viral DNA-what was that??
I wonder if they intended their new government to spend so much time and money providing and regulating health care –most of which was not available or even imagined at that time?
Public vs Private-not a perfect Union
The United States’ healthcare system combines public health efforts with mostly private delivery of health care. Usually they coexist side by side with some but infrequent interaction.
The public health emergency created by the pandemic forced them into a “union” that quickly became politicized, and unfortunately diminished the effectiveness of the response.
But despite the lack of coordination and cooperation between all levels of government and private citizens, our health care professionals, in both public health and private medical practice stayed true to their calling. Many risked their own lives to care for COVID-19 victims. Others sacrificed time and finances to lead the pandemic response in their communities and on social media- maybe not perfectly, but definitely UNITED in resolve to lead, help, and heal their fellow citizens through this unprecedented health emergency.
Let’s celebrate!

Sharing and celebrating the HEART of health
Dr. Aletha