updated April 21, 2025
I originally wrote this post during the COVID-19 pandemic. Now in 2025 we have new but not necessarily less significant concerns.
Healthwise, measles has made a resurgence in humans. Bird flu, H5N1 flu virus, is rampant throughout animals and threatens to jump into humans.
The world is in an economic crisis due to tariffs and a trade war. And wars in the Middle East, Eastern Europe, and many other places threaten the safety and lives of millions.
So use this advice originally offered to manage pandemic anxiety to manage concerns about the world situation today. Because let’s face it, there will always be something to worry about.
The original 2020 post
Even physicians feel stressed and uneasy about the COVID-19 pandemic, maybe more so than others. We’re supposed to be the ones with the answers to our patients’ questions and have the means to help them.
One of my collagues read an article about dealing with this stress, and to decrease our stress from he shared it in an email, with some edits.
So I am sharing it here. I have added a few of my thoughts and some references, as well as a link to the original article from CNNhealth.
Limit the frequency of your updates, including social media
With one of my patients, I suggested allowing herself one news check-in for 30 minutes each morning.
Choose a frequency and a time that works for you. But why stop there?

Consider a social media sabbatical. Give it a week and see how you feel. Taking the apps off your phone or tablet helps keep you accountable.
Name your fears
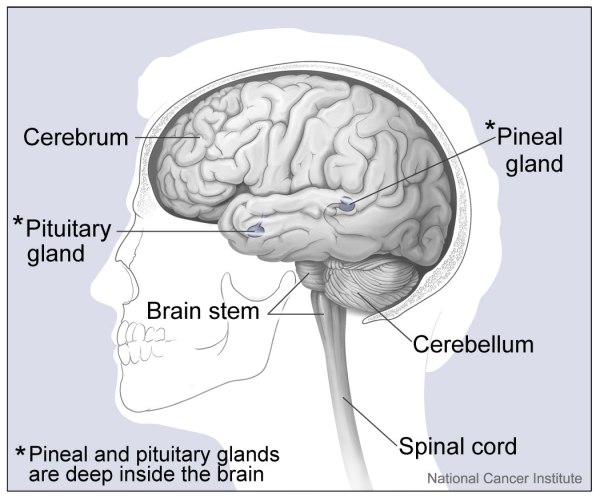
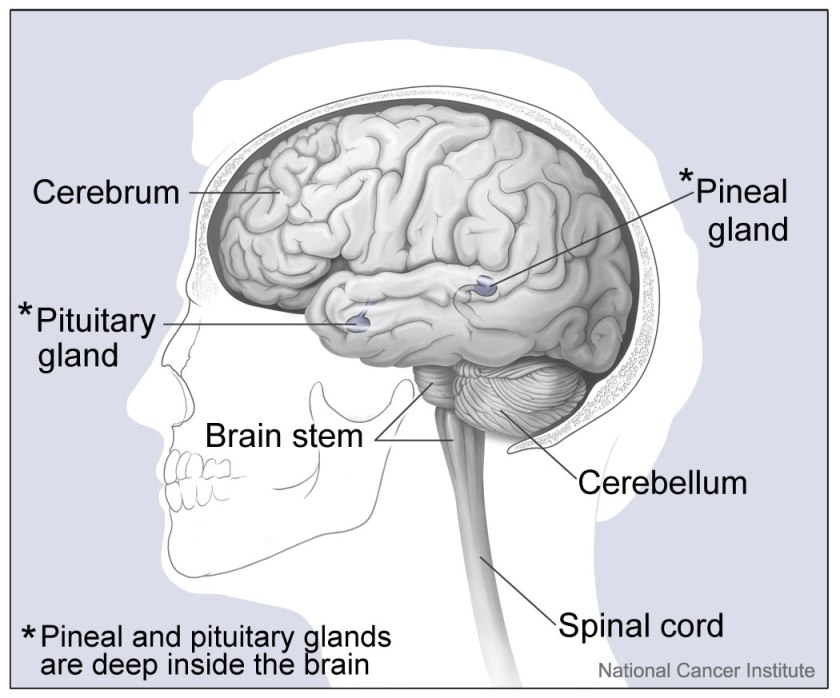
Recognize that we all have a negativity bias hard-wired into our brains. It’s a leftover evolutionary tool that helped keep our caveman and hunter-gatherer ancestors alive.
Unfortunately, it overestimates the likelihood that something tragic will befall us, and underestimates our capacity and resources to cope.
Conversely, if you minimize or ignore the threat of the pandemic, ask yourself if you should take it more seriously. If your reactions don’t match those of others in your community, your fear may have driven you to denial.

Think outside yourself:
If/when you are feeling overly worried and anxious, and your thinking feels contracted and hopeless, turn your thoughts to how you can help someone else.
This may be a child or other family member, a group of society that is at risk or marginalized at this time, or some of the groups at higher risk due to their occupations, age, or medical conditions.
When our thoughts turn to serving others, symptoms of worry, anxiety and depression lessen, and we feel better about ourselves.
And this does not have to be anything big, simply shifting to focus off of ourselves and onto someone else helps.

Seek support, but do it wisely
Don’t hesitate to ask for help if you need it. And that goes for us caregivers too.
We are not, and should not think of ourselves, as impervious to the various stressors, the disrupted routines and all of the uncertainty that is prevalent in the world right now.
Ask someone you can trust to be objective and rational, and not feed your worries or concerns.




Pay attention to your basic needs
Don’t get so wrapped up in thinking about the threats that you forget the essential, healthy practices that keep you physically well.
- Getting adequate sleep
- Keeping up with proper nutrition
- Getting outside as much as possible
- Engaging in regular physical activity
Practicing mindfulness, meditation, yoga, and spiritual disciplines will help center you in routines and awareness, and keep your mind from wandering into the dark and sometimes irrational unknown.

Don’t chastise yourself for worrying.
Again, this is part of our normal programming. And to help kids when they are scared, don’t just tell them everything is going to be alright.
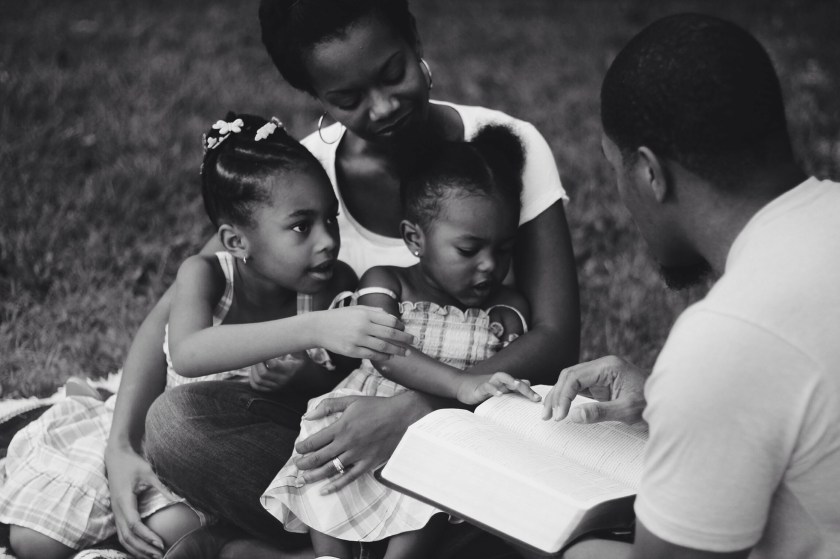
Let them know you hear their concerns and that you understand where they are coming from. And THEN give them evidence and reasoning for the opposite side of the worry equation.
Acknowledge their fears, and validate them… And then do the same for yourself.
This post was adapted from this article on CNNhealth
How to keep coronavirus fears from affecting your mental health
Thanks to my guest writer-Dane Treat, M.D.
Dr. Treat graduated from the University of Oklahoma medical school, although a couple of decades later than I did. He completed residency at Good Samaritan Family Practice in Phoenix, where he lives and practices now. He also completed a Sports Medicine fellowship. He is a student of Mindfulness-based Stress Reduction. He wisely married a Mayo Clinic trained gastroenterologist, and they are the proud parents of a daughter.

If you are depressed and thinking about or planning suicide, please stop and call this number now-988
988lifeline.org
SUICIDE AND CRISIS LIFELINE. CALL.TEXT.CHAT
Exploring the HEART of Health
I’d love for you to follow this blog. I share information and inspiration to help you transform challenges into opportunities for learning and growth.
Add your name to the subscribe box to be notified of new posts by email. Click the link to read the post and browse other content. It’s that simple. No spam.
I enjoy seeing who is new to Watercress Words. When you subscribe, I will visit your blog or website. Thanks and see you next time.